Pediatric Cancer Through A Precision Medicine Perspective
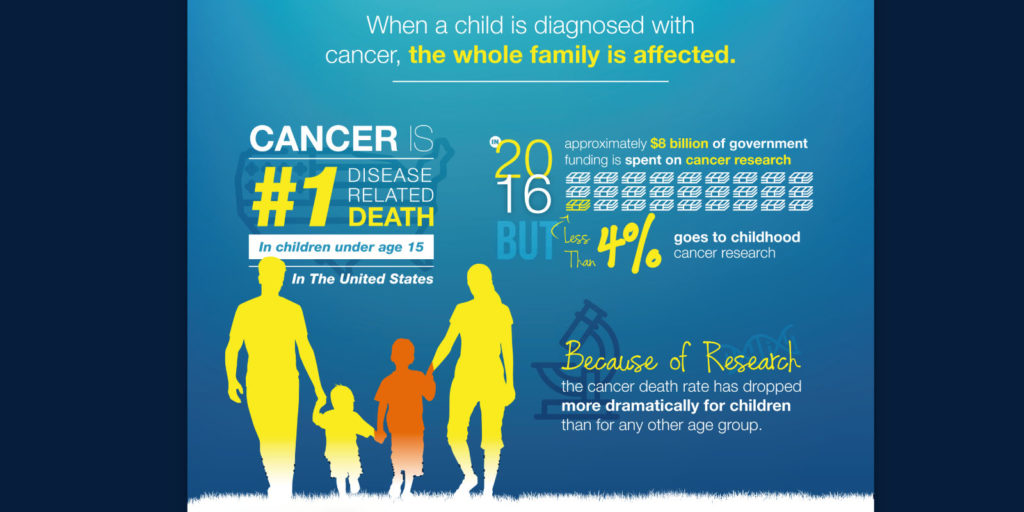
Despite the fact that pediatric cancer death rates have decreased and survival rates increased over the past decades as a result of major advances in cancer treatment, cancer continues to remain a leading cause of death among children.
According to the National Cancer Institute, in 2017, an estimate of 10,270 new cases of pediatric cancer will be diagnosed in the United States. The most common types of cancers diagnoses being: leukemia, brain and spinal cord tumors, lymphomas, and sarcomas. An estimate of 1,190 children is expected to die this year from this disease. [1]
The exact causes of what leads to pediatric cancer still remain unclear but continuous research efforts have made us exceptionally good at finding new information and novel methods of treatment; and while we might not know everything we know enough to continue the fight against pediatric cancer.
So here is what we know about pediatric cancer
Pediatric cancers are not the same as adult cancers
Both, pediatric and adult cancers arise from genetic mutations that lead to an uncontrollable growth of cells that are not “healthy”, thus, threatening the normal function of the body.
How far it spreads and how it is treated is dependent on the type of cancer, and the types of cancer that affect children are different from those that affect adults.
Biologically, cancers in children are different from those in adults primarily due to the type of cell from which it originates.
Adult cancers, such as breast, lung, and colorectal cancer, more often than not develop from epithelial tissue- cells that cover or line bodily surfaces and cavities. Conversely, pediatric cancers, including sarcomas and leukemia, develop often from immature pluripotent cells constituting non-ectodermal tissues such as bone marrow, lymph glands, bone, brain nerves, and muscle. [2]
In addition, the driving mechanisms are simpler. Pediatric cancers have fewer mutations instead of the dozens that may be present in adult cancers. These mutations almost exclusively occur in rapidly dividing tissues and greatly disrupt cell functions.
Pediatric cancers are more likely to develop due to genetics- inherited mutations passed from the parent to the child- or acquired during fetal development events. In contrast, adult cancers typically result from an accumulation of mutations that, in combination with external factors such as smoking or sun overexposure, later cause disease.
Children are not treated the same way as adults
Most adult cancers grow slowly enough that they can be monitored periodically, but pediatric cancers proliferate at terrifying speeds because of the tissues in which they develop. For this reason, when compared to adults, cancer is usually found at an advanced stage in children and require an immediate course of action.
Treating pediatric cancer shares some similarities to treating adult cancer. Chemotherapy, radiation therapy, immunotherapy, surgery, and stem cell transplants are still available and widely used methods of treatment for both categories of patients. But, considering that children’s bodies are unique and biologically different from adults (lung, liver or kidney functions are not considered fully mature until 15 years of age) some treatments or medicines for adults cannot be given to them; therefore, the amount of treatment available is limited, the type of treatment and the dosage need to be tailored to a more personal level.
Precision medicine as a novel treatment for pediatric cancers
The use of surgery, chemotherapy, and radiation therapy are still considered standard treatments for pediatric cancer. This is simply because they are effective at targeting cancers that arise in rapidly proliferating tissue, so by putting an abrupt stop to the rapid cell growth, we can observe a fast response and in a striking fashion. But, while the use of this standard treatments if effective at meeting the needs of an estimated 80% of children, there is still 20% of children with unique cancer characteristics.
By adopting a “precision medicine” approach in the area of pediatric cancer, we may attempt to identify a targeted therapy option for the remaining 20% of patients whose needs are unmet using standard cancer treatments and at the same time reduce the risk of treatment resistance and long-term deleterious effects.
Months or years after successful treatment completion severe side effects have been observed in pediatric cancer survivors: damage to organs such as the heart and lungs, stunted growth and development, infertility, and an increased risk of secondary cancers are the consequences of standard cancer treatments. [3]
The idea of precision medicine is not a new concept in pediatric oncology, but is not fully embraced. Genomic testing is already done to diagnose and assess many pediatric cancers. This is helpful in determining and designing treatment personalized treatments, but it sometimes may not be enough. A comprehensive dataset developed by a multi-institutional team, including the Dana-Farber/Boston Children’s Cancer and the Blood Disorders Center have helped provided further insight to the fight against cancer and where precision medicine stands in the matter.
The dataset, containing genomic profiles of known and previously-unknown gene mutations across six types and 49 subtypes of pediatric tumors, reveals that all tumors in a subtype do not always arise from the exact same genetic mutations. [4] This makes heterogeneity highlights the need for a higher level of treatment customization.
Because developing new regimens that will benefit patients with unique molecular profiles is constrictive- due to the lack of time knowledge, and resources- the idea of embracing personalized combination therapy of existing drugs appears more enticing. By creating a unique combination of treatment modalities that work synergistically, we are able to target each unique abnormality from a different angle and with a distinct and more appropriate mechanism of action. Personalized combination therapy then results in the ability to give an optimal dose and reduce long-term
and toxic side-effects while greatly improving a child’s quality of life.
Challenges to precision medicine in the area of pediatric cancer
Still, the embrace of precision medicine in pediatric cancer has been slow and challenging.
Until now, researching actionable targets in adult tumors have been the focal point of most pharmaceutical efforts. But pediatric cancer patients rarely benefit from these discoveries due to the limited overlap of genetic abnormalities occurring in adult tumors.
In addition, pediatric cancers have been observed to have fewer mutated genes compared to adult cancers, as a result, researchers have generally few genes to focus on, making targetable mutations in pediatric cancers rare.
A small number of patients and safety concerns in young children have been a challenge as well.
Pediatric cancer is rare- accounting for 1% of all cancers diagnosed. The small number of patients creates for a small population to study, a result, only a small subset of the potential drug will ever be studied. Currently, few targeted drugs are available to children in either approved or experimental form, and with the limited number of clinical trials, gathering critical information, such as age requirements, appropriate formulations, safety, and effectivity, comes to a crawling pace.
Fortunately, from the start, pediatric oncologists have created a culture of collaboration and sharing. Thanks to the sharing of information a larger number of researchers are able to contribute with new insights, insights that increase our knowledge and equips us with the necessary weapons in the fight against cancer.
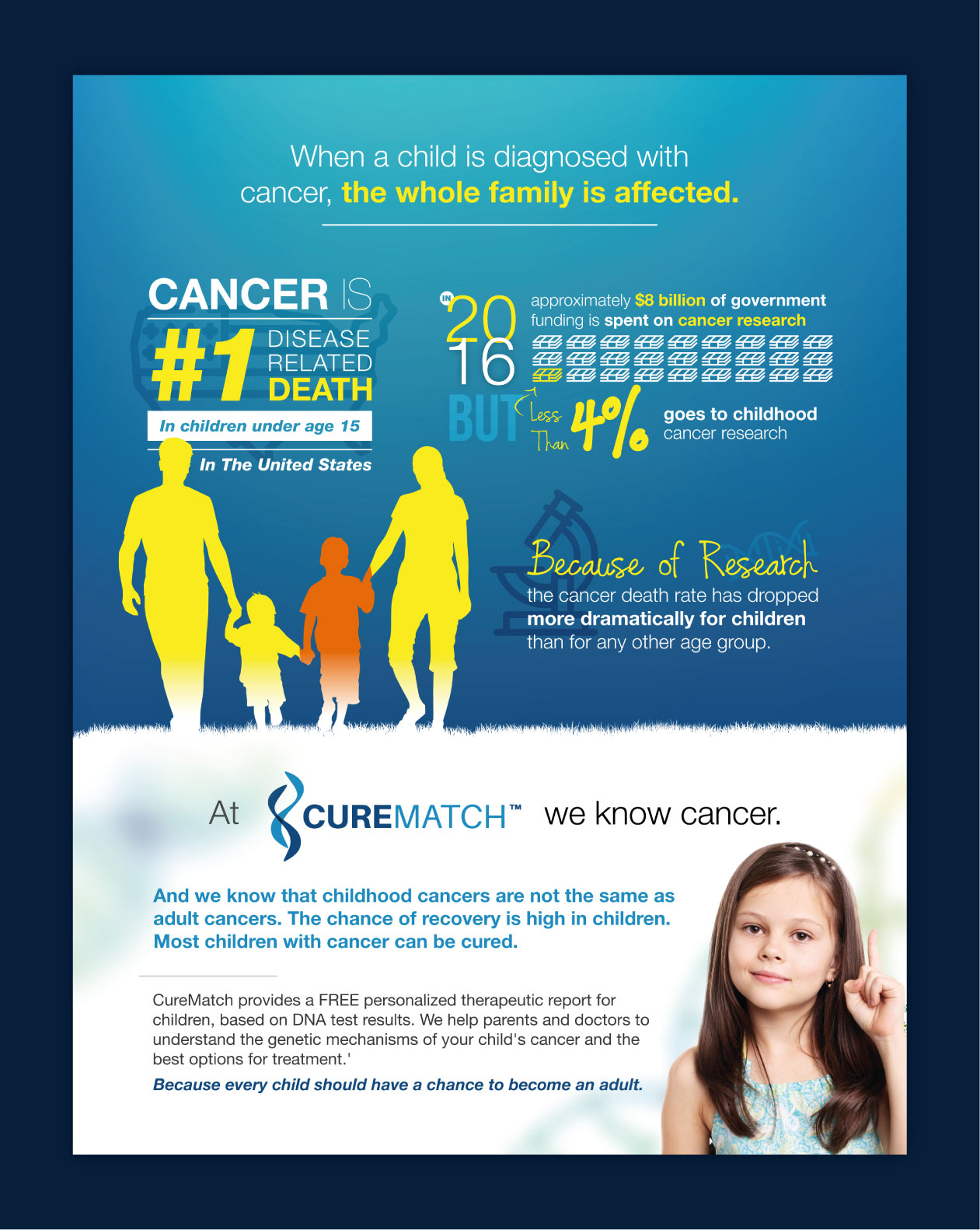
CureMatch takes pediatric cancer seriously
For CureMatch, children are the ones with the most life to lose and so we take this matter seriously.
We are working hard to provide a decision support system to guide clinicians, oncologists and pediatric cancer teams around the globe to the most effective combination therapy regimens.
Treatment begins with genetic testing of the tumor and through analytics, our database then sifts through all possible options to determine the most effective regimen personalized for each individual patient.
In joining the fight against pediatric cancer CureMatch offers this personalized service free of charge to children.
Author: Luis Pablos
REFERENCES
[1] Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA: A Cancer Journal for Clinicians 2017; 67(1):7-30.
[2] Institute of Medicine (US) and National Research Council (US) National Cancer Policy Board; Hewitt M, Weiner SL, Simone JV, editors. Childhood Cancer Survivorship: Improving Care and Quality of Life. Washington (DC): National Academies Press (US); 2003. The Epidemiology of Childhood Cancer.
[3] Childhood Cancers. NIH. https://www.cancer.gov/types/childhood-cancers
[4] Genomic Profiling of a Large Set of Diverse Pediatric Cancers Identifies Known and Novel Mutations across Tumor Spectra. Katherine A. Janeway et al. Res January 9 2017 DOI: 10.1158/0008-5472.CAN-16-1106