Breast Cancer: Paving The Way For Personalized Combination Therapy
Breast Cancer: Paving the Way for Personalized Combination Therapy
The concept of ‘Personalized Medicine’ has gained momentum in oncology over the past decade, as progress made in molecular biology now enables more precise definition of the characteristics of individual patients. As the benefits of using of tumor profiling to support advanced treatment options such as targeted therapy and immunotherapy have become recognized, it is now apparent that use of combinations of drugs to target molecular aberrations is the next frontier in oncology.
Throughout the evolution of cancer treatment, one specific pathology has traditionally been on the leading edge: breast cancer. Today we once again find breast cancer to be in this position – as a pioneer for new advances in personalized combination therapy.
It all started in 1896, when the British surgeon George Beatson first described the stimulating effect of a female circulating substance (later called estrogen) on breast tumor development. His work provided a foundation for the modern use of anti-hormone therapy in oncology: in 1977, the breakthrough anti-estrogen tamoxifen (NOVALDEX®) was approved by the FDA for the treatment of advanced breast cancer. Simultaneously, several studies underlined the importance of estrogen receptor (ER) to better stratify patients who benefit from anti-estrogen therapies (i.e., patients with ER-positive tumors) from those who do not benefit and only suffer from unnecessary side effects of the drug (i.e., patients with ER-negative tumors). Today, the evaluation of ER expression level is a mandatory prerequisite for adequate management of breast cancer, and may therefore be considered as one of the first models for molecular-driven medicine.
Another important milestone in the care of breast cancer patients was the approval, in 1998, of the drug trastuzumab (HERCEPTIN®). Previous research showed that adding the monoclonal antibody to chemotherapy dramatically increases survival for women with advanced breast cancers in which a protein called Her-2 is over-produced.
Dysregulation of the cell cycle is a classic hallmark of cancer growth, and is largely observed in breast tumors. Therefore, re-establishing cell cycle control has emerged as an attractive option in the development of personalized therapy, and such molecules have shown extended response in newly diagnosed, as well as advanced and resistant, breast cancer patients.
While long considered individually, these three molecular drivers of breast oncogenesis (ER, Her2, and cell-cycle) may also be used together to suggest corresponding ‘a la carte’ drug combinations. Based on this concept, the FDA recently approved several therapeutic regimens that demonstrated superior safety and efficacy to monotherapies in breast cancer care. This approach has been shown to successfully overcome monotherapy drug resistances in other diseases such as HIV. A summary of combinations acknowledged by the FDA for the care of breast cancer is provided in the table below:
THERAPEUTIC REGIMENS APPROVED BY THE FDA FOR THE TREATMENT OF BREAST CANCER
| A patient presenting a tumor that is | Will benefit from: |
| ER-positive, Her2-positive | a combination of anti-estrogen and Her2 blocker[1] |
| ER-positive, Her2-negative | |
| with cell-cycle altered | a combination of anti-estrogen and cell-cycle blocker letrozole (FEMARA®) and palbociclib (IBRANCE®) |
| with cell-cycle unaltered | an anti-estrogen alone |
| ER-negative, Her2-positive | a Her-2 blocker alone[2] |
The remaining category of tumors – tumors that are negative for both estrogen and Her2 receptors (not shown in the table) – concerns 15 to 20% of all diagnosed breast cancers and is still considered to be a therapeutic challenge. However, this heterogeneous subgroup is composed of at least 4 to 6 definable molecular subtypes that may be sensitive to treatments targeting other cellular processes, such as PARP (poly ADP-ribose polymerase) inhibitors, VEGF (vascular endothelial growth factor) inhibitors, or EGFR (epidermal growth factor receptor) inhibitors, as well as suitable cytotoxic chemotherapy. These subtypes of breast cancers are therefore prime candidates for the development of new personalized combination therapy options, and are under investigation for what is seen as the ultimate ‘Holy Grail’ in breast cancer research.
Overall, the advances in therapeutic management of breast cancer demonstrate how, by using a limited set of pharmacology classes and associating them in a ‘mix-and-match’ combination by taking into account the molecular fingerprint of each patient, health care specialists have managed to proficiently improve patient outcomes. Just as breast cancer has served as a proving ground for new treatment options in the past, we expect these positive results to pave the way for broader use of personalized combination therapies throughout oncology.
-Amelie Boichard, Ph.D.
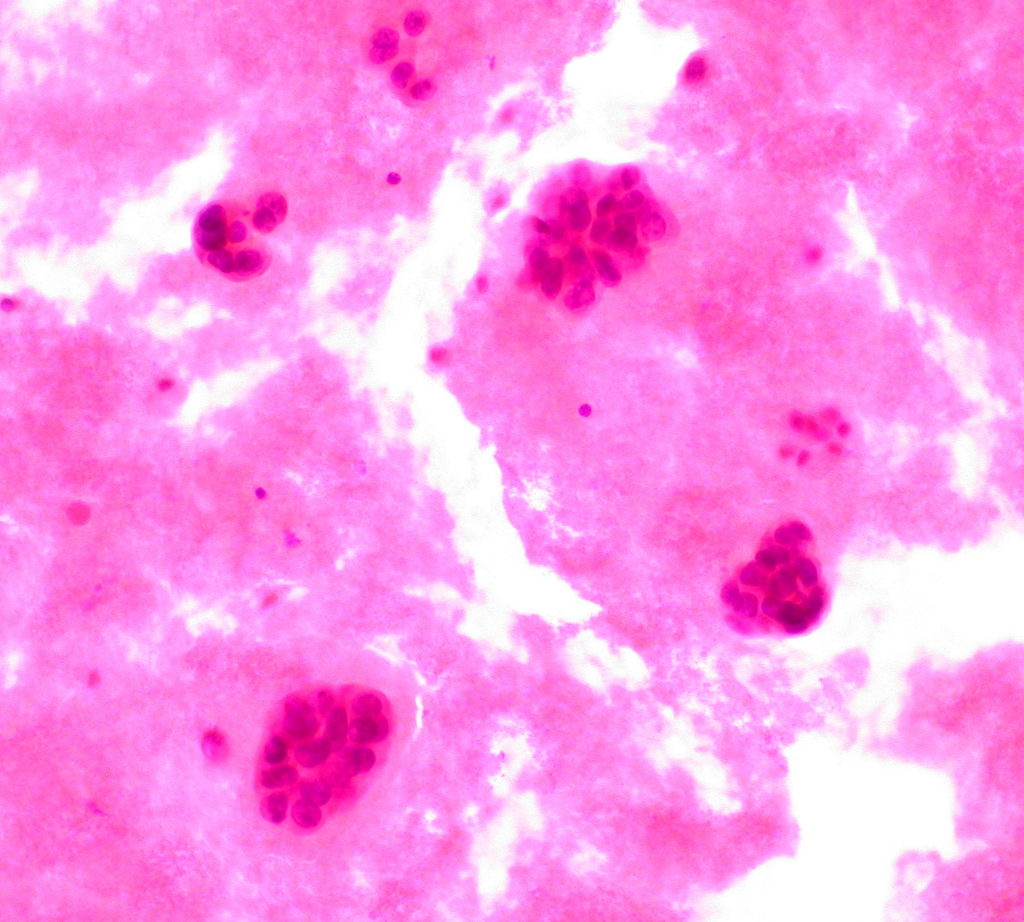
“Metastatic Breast Cancer in Pleural Fluid” flickr photo by Ed Uthman shared under a Creative Commons License.
[1] Several phase II clinical trials studying the benefit of a combination of an anti-estrogen with a Her2 blocker and a cell-cycle blocker are currently in progress for patients carrying an ER-positive / Her2-positive / cell-cycle altered tumor.
[2] Several phase II clinical trials studying the benefit of a combination of a Her2 blocker with a cell-cycle blocker are currently in progress for patients carrying an ER-negative / Her2-positive /cell-cycle altered tumor.